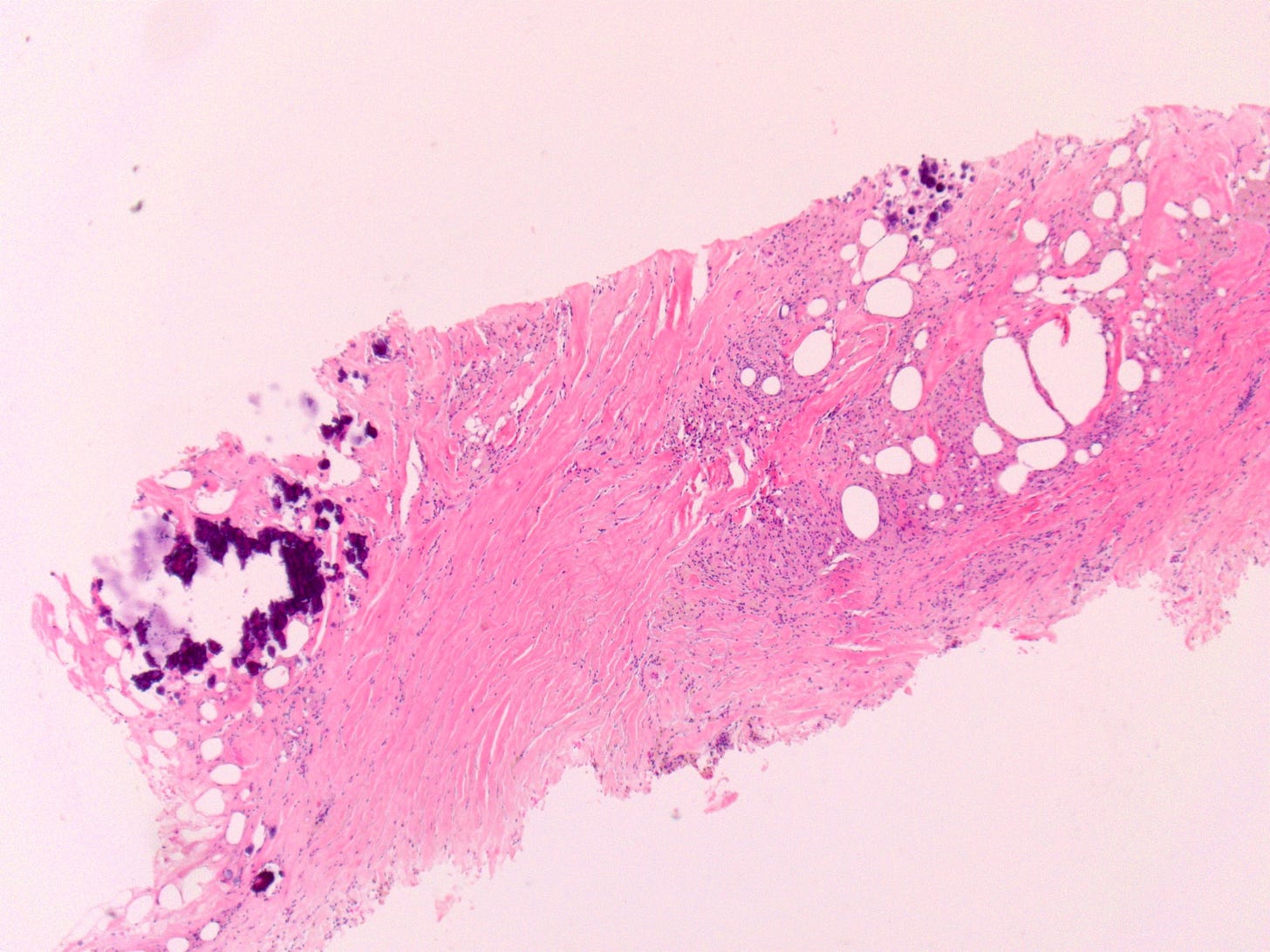
Fat necrosis in the breast parenchyma is a benign, non-suppurative inflammatory process resulting from injury to adipose tissue. The histologic appearance evolves over time, with calcifications typically being a later stage feature.
Histologic Features:
Early/Acute Phase:
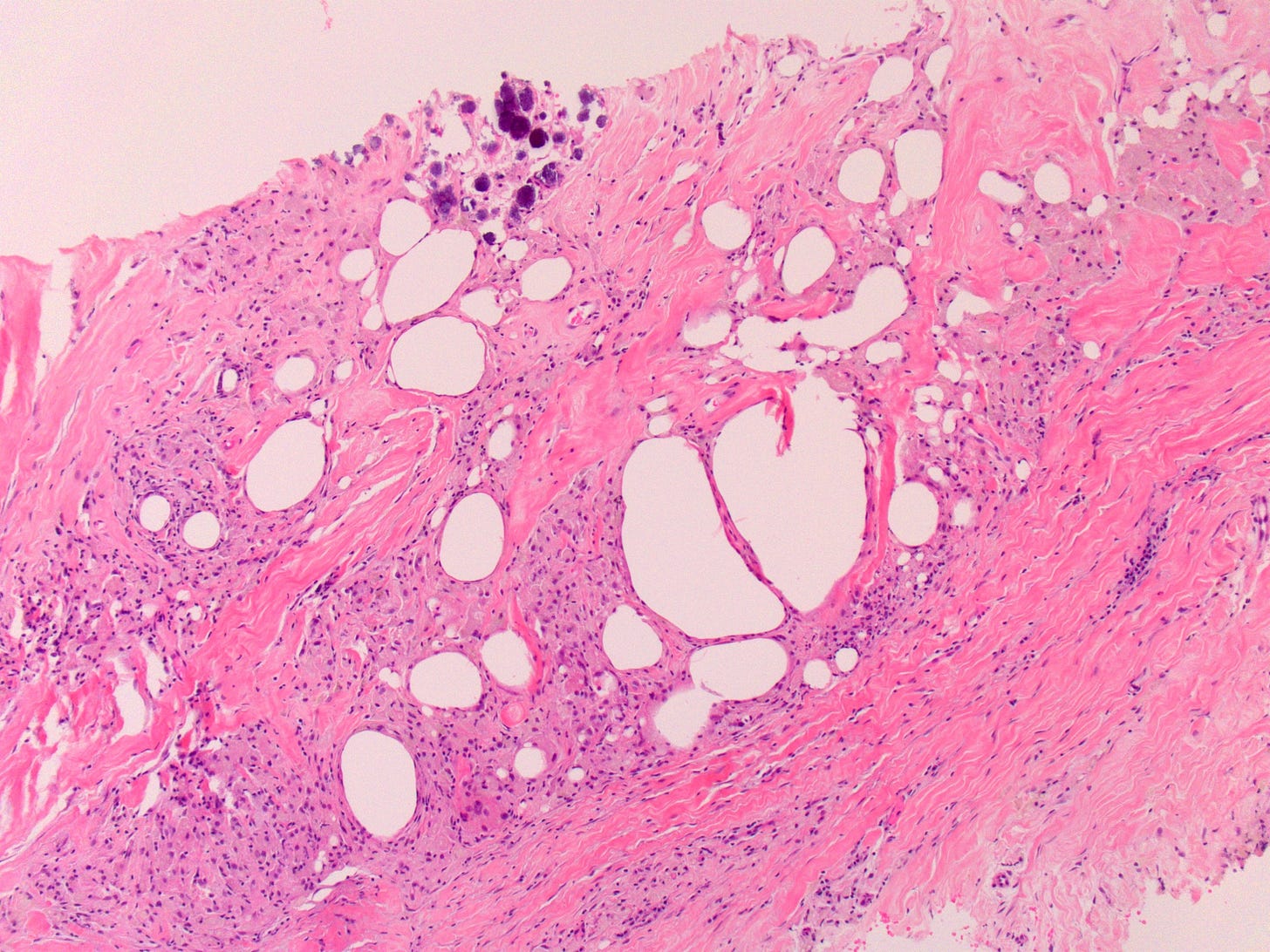
Disruption of adipocytes with release of neutral fat, forming cytoplasmic vacuoles and lipoid cysts (oil cysts) within the tissue.
Influx of acute inflammatory cells (neutrophils) and hemorrhage.
Subacute/Organizing Phase:
Multinucleated giant cells (foreign body type) may be seen, often surrounding lipid droplets.
Lymphocytes and plasma cells contribute to the chronic inflammatory infiltrate.
Developing fibrosis around the necrotic fat and inflammatory cells.
Late/Chronic Phase:
Predominance of fibrosis, which can appear as dense scar tissue, sometimes with architectural distortion.
Persistent oil cysts of varying sizes, often with calcified walls.
Residual inflammatory cells, particularly foamy macrophages and giant cells, may still be observed within and around the fibrotic areas.
Hemosiderin deposition may be present from prior hemorrhage.
Calcifications: These are a hallmark and can vary in morphology. They often appear as:
Dystrophic calcification: Irregular, coarse, amorphous deposits.
Rim-like or "eggshell" calcifications: Curvilinear calcifications outlining the walls of oil cysts.
Finer, punctate calcifications may also be present, which can sometimes mimic malignancy on imaging, necessitating biopsy for definitive diagnosis.
In summary, fat necrosis with calcifications is characterized by a spectrum of changes including necrotic fat, lipid-laden macrophages, multinucleated giant cells, fibrosis, and varying patterns of calcification.
This post created in collaboration with AI tools.